INTRODUCTION
Smoking is a recognized modifiable risk factor for many non-communicable diseases, and remains one of the biggest global public health challenges1,2. Previous studies report a 20–30% smoking prevalence in western countries and a 12–47% smoking prevalence in Asian countries1,3-5. Recent data5,6 have shown that a total of 52 diseases are associated with smoking and over 7 million people die each year due to tobacco related diseases globally, including cardiovascular diseases, cancer, chronic obstructive pulmonary diseases, etc. The cost burden of tobacco smoking is high, 7.69 million (7.16–8.20) deaths and 200 million (185–214) disability adjusted life years (DALYs) in 2019 globally could be attributed to tobacco smoking1,7. Therefore, reducing smoking prevalence is an important healthcare task, and quitting smoking remains the crucial public health goal to save lives and reduce the burden of disease induced by tobacco smoke5.
The epidemic of non-communicable diseases (NCD) continues to rise unabated worldwide leading to approximately 40 million deaths annually, of which 42% of NCD deaths are premature8. Although the number of NCD deaths has increased in worldwide since 2000, the burden is greatest among people in low- and middle-income countries9. In the South-East Asia Region, NCD are responsible for 14.5 million of all deaths, and tobacco smoking directly contributes up to 14% of all NCD deaths in adults, which is expected to rise to 6.8 million in 2030 in low- and middle-income countries in the absence of robust action10. Evidence from existing literature indicate that tobacco smoking is closely related to NCD, the pooled prevalence of tobacco smoking among patients with hypertension and cancer is 12.9% and 18.7%, respectively11. Tobacco control is as an effective strategy to decrease the trend of the NCD epidemic. Therefore, encouraging smoking cessation can prevent the onset or progress of NCD and reduce mortality12.
Quitting tobacco smoking can lead to substantial health gains, even later in life13. The Framework Convention on Tobacco Control (FCTC) is the first evidence-based treaty to combat the tobacco epidemic and has elaborated efficient supply and demand reduction measures to address the tobacco menace14. Most smokers wish to quit and approximately 40% of them try to stop smoking for at least once each year, but quitting is challenging and only 3–5% of unaided attempts are successful 6 to 12 months later13,15. The most effective cessation strategy to help smokers quit is through expert behavioral support combined with cessation aids, but over 85% of globally smoking population does not have access to the comprehensive measures, which has also contributed to the low successful rate of smoking cessation16,17. Previous studies indicate that illness can be a powerful motivation to quit18, and advice on smoking cessation from doctors and other health professionals has been shown to improve quit rates and is highly cost-effective19. But evidence on the role of NCD in smoking cessation is still limited.
Smoking is a public crisis in China, with 320 million current tobacco smokers. Based on the Global Adult Tobacco Survey (GATS) implemented in 2010, tobacco related diseases caused nearly 1 million deaths among smokers in China20,21. Expenses from tobacco related diseases cost 9 billion US$, accounting for 1.5% of the total national healthcare expenditure in 2014 based on WHO estimation16,20-22. Due to the tobacco induced heavy diseases burden, China implemented the WHO FCTC in 2006, but made slow and limited progress on tobacco control20. For example, the prevalence of smoking in Beijing has only dropped from 23.4% in 2014 to 22.3% in 2019, and the smoking rate only decreased by 0.3% between 2017 and 2018 in Shanghai23,24. In order to reduce the smoking prevalence in China, exploring salient tobacco control policies to encourage current tobacco smokers to quit or prevent smoking, are crucial.
We conducted a cross-sectional study to evaluate the prevalence of non-communicable diseases among current smokers, and to explore how smoking cessation intention is influenced by NCD status among current smokers in Shanghai, China.
METHODS
Study design
During January to June 2021, we implemented this cross-sectional study in Songjiang and Fengxian districts in Shanghai. Songjiang district is located in the southwest of Shanghai with a population of 1.91 million in 2020, and Fengxian district is located in the southeast of Shanghai with a population of 1.14 million in 2020 (Figure 1). In this study, current smokers did not constitute a random sample of the entire smoking population in Shanghai, but was a convenience sample selected judiciously based on geographical representation25. The sample size, n, was calculated based on the formula for a cross-sectional study:
n = [μ2α/2 × p(1 - p)] / δ2,
with a prevalence, p, of NCD set at 30%, α=0.05, δ=10% of p, and a 15% non-response rate, a total of at least 1030 current smokers were required to be recruited in this study. Multistage sampling method was employed to recruit current smokers among the 15 sub-districts in Songjiang district and the 12 sub-districts in Fengxian district, Shanghai. detailed information for smoker recruitment by multistage sampling can be found in our previous published works25,26. A total of 1104 smokers completed the interview and were included in the final data analysis. This study conformed to the principles embodied in the Declaration of Helsinki, and informed consent was signed by each participant. This study was reviewed and approved by Review Board of Shanghai Skin Diseases Hospital of Tongji University.
Data collection
We employed an electronic questionnaire for data collection25,26. The electronic questionnaire has an audio record function which allows data entry quality inspection and is convenient for paperless data input. The questionnaire included four parts. Part A was the demographic feature covering the age of smokers, gender, residency status, marital status, occupation, education level and income. Part B covered 8 types of NCDs including respiratory system (RS) related NCD (chronic bronchitis, chronic obstructive pulmonary diseases and asthma) and non-RS-related NCD (hypertension, type 2 diabetes, cancer, cerebroinfarction, and coronary heart diseases). Part C includes tobacco consumption information (age of smoking initiation, retail price of daily consumed tobacco, smoking cessation history, etc.). Part D covered information on plan to quit tobacco smoking in a year, and personal contact information of the investigator.
Definition and index calculation
In this study, a current smoker was defined as a person who smoked ≥100 cigarettes in a lifetime and still smoked at the time of investigation25,26. Smoking duration was defined as the time interval between investigation time and smoking initiation time in current smokers25, and then classified it into <20 and ≥20 years. We defined smoking intensity as the number of cigarettes smoked per day and then categorized it as <20 and ≥20 cigarettes/day. In this study, age of current smokers was classified into <45 years and ≥45 years, and marital status was divided into unmarried, married and divorced/widows. Education level was recorded as completed years of schooling and classified into three categories: ‘junior high school and lower’ (1–9 years of schooling), ‘senior high’ (10–12 years of schooling), and ‘college and higher’ (over >12 years of schooling). Occupation was classified as laborer, professional, and unemployed. Individual monthly income was categorized into three groups: <5000, 5000–10000, and >10000 RMB (1000 Chinese Renminbi about 140 US$). The 7 types of NCD were classified into respiratory system (RS) related NCD and non-RS-related NCD25,26.
Statistical analysis
In this study, SAS 9.4 (SAS institute Inc) was applied for data analysis. Quantitative data are presented as means and standard deviations (SD) with normal distribution, and as median and interquartile range (IQR) with skewed distribution. We applied Student’s t-test or Mann-Whitney U tests to examine the difference between quantitative variables with normal or skewed distribution, respectively. Qualitative variables were described as frequency counts (n) and percentage (%), and a chi-squared test was used to test differences between groups. The odds ratio (OR) and 95% confidence interval (95% CI) was calculated by binary logistic regression to explore the association between NCD prevalence and smoking cessation intention among current smokers, with the adjustment of potential confounders identified by directed acyclic graphs (DAGs). In this study, age, marital status, and sex were identified by DAG as potential confounders for all current smokers with NCD, age, sex and education level identified by DAG as potential confounders for current smokers with RS-related NCD, and age, marital status, education level and sex were identified by DAG as potential confounders for current smokers with non-RS-related NCD. Figures were produced to show differences in smoking duration, smoking intensity and smoking cessation attempts among current smokers for different demographic characteristics. We set α=0.05, and differences with a p<0.05 were considered to be statistically significant.
RESULTS
The age of the 1104 current smokers ranged from 18 to 73 years, with an average age of 43.6 years; 83% of current smokers were males, 85% of smokers were married and 63% had an education level of college and higher; 45.5% and 32.5% of smokers were professionals, and laborers, respectively, while 22.0% were unemployed. Nearly 75% of smokers had an individual monthly income ≥5000 RMB, and 85% of smokers were local residents. Table 1 shows that male current smokers were older, had a higher proportion of married status, had a lower percentage of unemployment, and an individual monthly income <5000 RMB.
Table 1
Demographic characteristics among current smokers in rural areas of Shanghai, China, 2021 (N=1104)
Prevalence of NCD among current smokers
Approximately 22% of smokers had at least 1 type of non-communicable disease, with 17.8% non-RS-related NCD and 6.6% for RS-related NCD. The prevalence of NCD comorbidity among current smokers was 13.9% for hypertension, 6.0% for chronic bronchitis, 3.4% for type 2 diabetes, 2.1% for cancer, 0.8% for chronic obstructive pulmonary disease, 0.6% for asthma and 0.5% for coronary heart diseases. Table 1 shows that male current smokers had a high proportion of at least 1 type of non-communicable disease, both for RS-related NCD and non-RS-related NCD, in comparison with female smokers.
Tobacco smoking among current smokers with NCD
The mean value of the tobacco smoking initiation age was 21.2 ± 4.9 years, and the median value of smoking duration was 14 years (IQR: 20–37). The percentage of smoking duration ≥20 years was 58.9%. The 1104 current smokers consumed 15 cigarettes (IQR: 10–20) per day on average, and spent 700 RMB (IQR: 300–1000) each month on average. Over 60% of smokers had smoking intensity <20 cigarettes/day, and 47.9% of current smokers had attempted to quit smoking previously but relapsed. In comparison with smokers without NCD, smokers with NCD had longer years of tobacco smoking, the proportion of smoking duration ≥20 years (76.8% vs 53.9%) and smoking intensity ≥20 cigarettes per day (47.3% vs 37.3%) was higher, and they spent more RMB on tobacco purchase. Differences between smokers with or without RS-related NCD, and smokers with or without non-RS-related NCD were in line with the findings among smokers with or without NCD (Table 2).
Table 2
The smoking intensity, smoking duration, tobacco expenses, and smoking cessation attempt among current smokers in rural area of Shanghai, China, 2021 (N=1104)
| Variables | Total smokers (n=1104) n (%) | Smokers with NCD | Smokers with RS-related NCD | Smokers without RS-related NCD | |||
|---|---|---|---|---|---|---|---|
| Yes (n=241) n (%) | No (n=863) n (%) | Yes (n=73) n (%) | No (n=1031) n (%) | Yes (n=197) n (%) | No (n=907) n (%) | ||
| Age of tobacco smoke initiation, mean ± SD | 21.2 ± 4.9 | 21.2 ± 4.6 | 21.2 ± 4.9 | 20.7 ± 5.0 | 21.2 ± 4.9 | 21.6 ± 4.7 | 21.1 ± 4.9 |
| Years of tobacco smoking†ǂ‡, median (IQR) | 14 (20–37) | 20 (28–37) | 11 (21–28) | 31 (20–40) | 22 (13–29) | 28 (21–36) | 21 (12–28) |
| Smoking duration (years)†ǂ‡ | |||||||
| <20 | 454 (41.1) | 56 (23.2) | 398 (46.1) | 16 (21.9) | 438 (42.5) | 43 (21.8) | 411 (45.3) |
| ≥20 | 650 (58.9) | 185 (76.8) | 465 (53.9) | 57 (78.1) | 593 (57.5) | 154 (78.2) | 496 (54.7) |
| Daily consumed cigarettes on average†ǂ‡, median (IQR) | 15 (10–20) | 15 (10–20) | 15 (8–20) | 20 (12–20) | 15 (8–20) | 15 (10–20) | 15 (8–20) |
| Smoking intensity (cigarettes/day)†ǂ‡ | |||||||
| <20 | 668 (60.5) | 127 (52.7) | 541 (62.7) | 35 (47.9) | 633 (61.4) | 111 (56.4) | 557 (61.4) |
| ≥20 | 436 (39.5) | 114 (47.3) | 322 (37.3) | 38 (52.1) | 398 (38.6) | 86 (43.6) | 350 (38.6) |
| Monthly expense on tobacco purchase†ǂ, median (IQR) | 700 (300–1000) | 750 (400–1000) | 600 (300–1000) | 1000 (500–1200) | 700 (300–1000) | 700 (400–1000) | 700 (300–1000) |
| Smoking cessation attempt | |||||||
| Yes | 529 (47.9) | 126 (52.3) | 403 (46.7) | 40 (54.8) | 489 (47.4) | 105 (53.3) | 424 (46.8) |
| No | 575 (52.1) | 115 (47.7) | 460 (53.3) | 33 (45.2) | 542 (52.6) | 92 (46.7) | 483 (53.2) |
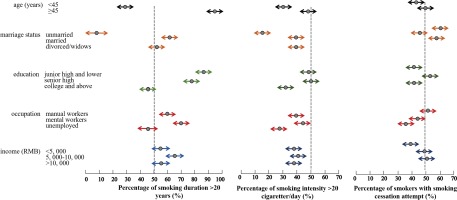
Figure 2 shows that smokers aged ≥45 years had higher percentage of smoking duration ≥20 years, smoking intensity ≥20 cigarette/day, and tobacco smoking quit attempt. Unmarried smokers had lower percentage of smoking duration ≥20 years and smoking intensity ≥20 cigarette/day, but higher percentage of quit attempt. Smokers with college and higher education had lower percentage of smoking duration ≥20 years, smoking intensity ≥20 cigarette/day and lower quit attempt. Professionals with tobacco smoking had higher percentage of smoking duration ≥20 years and smoking intensity ≥20 cigarette/day, but lower quit attempt (Figure 2).
Smoking cessation intention among current smokers
In this study, 41.8% (462/1104) of current smokers had intention to quit smoking in a recent year. The percentage of smoking cessation intention was higher in current smokers with at least 1 type of non-communicable disease, as well as RS-related NCD and non-RS-related NCD. Smokers aged <45 years (46.5%) had higher percentage of smoking cessation intention than those aged <45 years (38.1%), and female smokers (45.3%) had higher percentage of smoking cessation intention than male smokers (25.3%), the differences were all statistically significant (p<0.05). Smokers with an education level of college and higher (39.5%), had lower cessation intention than those with senior high (48.5%), the difference was statistically significant (p<0.05). Smokers with married status, with 5000–10000 RMB monthly income, and smoking intensity ≥20 cigarettes per day had lower smoking cessation intention, but was not statistically significant (Table 3).
Table 3
Percentage of smoking cessation intention among current smokers in rural areas of Shanghai, China, 2021 (N=1104)
[i] AOR: adjusted odds ratio. RS: respiratory system. RMB: 1000 Chinese Renminbi about 140 US$. Model 1: multi-variate logistic regression for prevalence of smoking cessation intention among current smokers with NCD, with the adjustment of age, marital status, and sex. Model 2: multi-variate logistic regression for prevalence of smoking cessation intention among current smokers with RS-related NCD, with the adjustment of age, sex and education level. Model 3: multi-variate logistic regression for prevalence of smoking cessation intention among current smokers with non-RS-related NCD, with the adjustment of age, marital status, education level and sex.
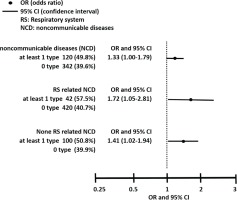
Logistic regression analysis demonstrated that current smokers with NCD had higher percentage of smoking cessation intention than those without NCD, with AOR equal to 1.33 (95% CI: 1.00–1.79) with the adjustment of potential confounding factors. Similarly, smokers with RS-related NCD as well as with non-RS-related NCD had higher percentage of smoking cessation intention than those without, with AOR of 1.72 (95% CI: 1.05–12.8) for smokers with RS-related NCD and 1.41 (95% CI: 1.02–1.94) for smokers with non-RS-related NCD (Table 3).
Figure 3 and Table 4 show the association between smoking cessation intention and NCD in each category. In comparison with smokers without NCD, current smokers with chronic obstructive pulmonary disease (COPD), coronary heart diseases, hypertension, and chronic bronchitis had higher prevalence of smoking cessation intention, the AORs were 26.9 (95% CI: 1.56–463.7), 18.3 (95% CI: 1.03–325.6), 1.66 (95% CI: 1.18–2.33) and 1.97 (95% CI: 1.19–3.25), respectively. Smokers with diabetes, cancer and asthma also had higher prevalence of smoking cessation intention, but the difference was not statistically significant.
Table 4
The percentage of smoking cessation intention among current smokers with or without non-communicable diseases (NCD) in rural areas of Shanghai, China, 2021 (N=1104)
| Non-communicable diseases | Intention to quit in a year n (%) | AOR | 95% CI |
|---|---|---|---|
| Hypertension | |||
| Yes | 81 (52.60) | 1.66 | 1.18–2.33 |
| No | 381 (40.11) | 1 | |
| Chronic bronchitis | |||
| Yes | 38 (57.58) | 1.97 | 1.19–3.25 |
| No | 424 (40.85) | 1 | |
| Type 2 diabetes | |||
| Yes | 16 (43.24) | 1.07 | 0.55–2.06 |
| No | 446 (41.80) | 1 | |
| Cancer | |||
| Yes | 10 (43.48) | 1.08 | 0.47–2.46 |
| No | 452 (41.81) | 1 | |
| Chronic obstructive pulmonary disease | |||
| Yes | 9 (100) | 26.9* | 1.56–463.7 |
| No | 453 (41.37) | 1 | |
| Coronary heart diseases | |||
| Yes | 6 (100) | 18.3* | 1.03–325.6 |
| No | 456 (41.53) | 1 | |
| Asthma | |||
| Yes | 4 (57.14) | 1.86 | 0.41–8.35 |
| No | 458 (41.75) | 1 | |
DISCUSSION
Tobacco smoking increases risk for many diseases and the associated deaths, and smoking is a modifiable behavior27,28. Previous studies indicate that tobacco use increases the risk of coronary heart diseases by 2- to 3-fold, stroke by 1.5-fold, COPD by 1.4-fold and lung cancer by 12-fold29. In this study, approximately 22% of smokers had at least 1 type of non-communicable disease; the prevalence of NCD was 13.9% for hypertension, 6.0% for chronic bronchitis, 3.4% for type 2 diabetes, 2.1% for cancer, 0.8% for chronic obstructive pulmonary disease, 0.6% for asthma and 0.5% for coronary heart diseases, these findings are in line with previous studies4,30. The adult tobacco survey in 2013 enrolled 175386 residents in China and indicated that the prevalence of hypertension, hypertriglyceridemia and hypercholesteremia was 30.4%, 7.2% and 18.0%, respectively, in male smokers, and 35.6%, 10.3% and 15.9% respectively, in female smokers, which were higher than among non-smokers4. Another investigation, implemented in 2017 in Shanghai, demonstrated that the prevalence of NCD among smokers ranged from 0.63% to 36.3%, and was obviously higher than in non-smokers for hypertension, coronary diseases and chronic bronchitis30. The determinants of NCD are multi-factorial, lifestyle and individual behavior change is crucial to reduce these risk factors31. Therefore, tobacco control could be a cost-effective strategy to decrease the trend of the NCD epidemic, especially among tobacco smokers.
Growing evidence indicates that most tobacco smokers have the intention to quit, and about 40% of smokers have tried to quit at least once each year13,15. In this study, the percentage of smoking cessation attempt was 47.9%, which was higher among smokers with NCD than those without NCD, but all relapsed; this might be mainly due to the heavy tobacco dependence among smokers, especially those with NCDs32. In this study, smokers with NCD had higher percentage of smoking duration ≥20 years and higher percentage of smoking intensity ≥20 cigarettes/day, indicating more severe tobacco dependence19. As a chronic addictive disease, tobacco dependence is hard to quit and most smokers experience relapse after smoking cessation32. Nicotine in tobacco smoke is one of the most addictive substances which can enter the brain within seconds and act on the mesolimbic reward pathway, this causes the release of dopamine and produces a mood elevated physiologic response that becomes highly addictive33. Meanwhile, withdrawal symptoms can last for 6 weeks or longer, which also contributes to smoking cessation relapse27.
Smoking cessation is the most powerful and cost-effective intervention, which improves the overall health and quality of life among smokers, especially those with NCD34. In this study, less than half of current smokers had intention to quit in a year, which was lower than the findings in previous studies15,19. The lower smoking cessation intention among smokers in this study indicated heavier nicotine dependence and lower awareness of smoking cessation benefits among current smokers in Shanghai. Health organizations should implement more health education and health promotion activities to advocate the benefits of smoking cessation and the harm of tobacco smoking among tobacco smokers. There is growing evidence that quitting smoking before the age of 40 years can reduce tobacco related mortality by 90%, and smoking cessation benefits people of all ages, regardless of smoking duration19. Meanwhile, Article 14 of the FCTC states counselling and psychological support as important measures to reduce tobacco dependence and increase cessation measure use, which can also be incorporated into smoking cessation measures in the future.
Illness can be a powerful motivation to quit among smokers18, and a Cochrane review that included 42 randomized clinical trials found that brief advice of a physician was associated with higher smoking cessation rates35. In this study, we noticed that the percentage of smoking cessation intention among smokers with NCD was higher than those without. In comparison with smokers without NCD, current smokers with COPD, coronary heart diseases, hypertension, chronic bronchitis had 26.9, 18.3, 1.7 and 1.9 times higher percentage of smoking cessation intention, respectively, and smokers with diabetes, cancer and asthma also had higher smoking cessation intention. In order to curb the high smoking prevalence and promote smoking cessation, it is crucial to pay special attention to smokers with NCD, providing professional smoking cessation counseling, psychological support and individualized treatment based on clinical setting can effectively improve the success rate of smoking cessation among them32,34.
In recent years, elevated evidence indicates that cognitive and behavioral therapy delivered by health professionals has a significant effect on quit rates; individual counseling improves long term quit rates by 40%31. Smoking cessation service in clinical settings should be a fundamental clinical responsibility and affords the chance to more efficiently and effectively assist cessation34. However, the availability of clinical setting consultation and physicians’ cessation services are extremely limited in China36. Studies demonstrate that <50% of physicians ask about patients’ tobacco use status, and only 30% of physicians think smokers will follow cessation advice they provided, and <7% of physicians provide tobacco cessation advice36. The possible barriers limiting the smoking cessation service include: 1) lack of time, 2) lack of confidence in addressing smoking cessation, 3) lack of training in smoking cessation treatment, and 4) outdated attitude toward tobacco addiction. Therefore, improving the utilization and availability of clinically based tobacco control measures is urgent to reach the under-served smoking population in China. We recommend health organizations and institutions should develop comprehensive smoking cessation programs in a clinical setting, and train physicians to implement them. Clinicians should treat tobacco status as a vital sign by asking all patients in each clinic visit, record their answers and provide brief counselling, professional guidance and medication assistance for smoking cessation, meanwhile, encourage those who do not smoke to continue healthy habits and never start smoking.
The Global Action Plan for Prevention and Control of NCD targets are to achieve 30% relative decrease in the prevalence of current tobacco use in persons aged >15 years, reduce premature mortality from NCD by 33% by 2030, and implementation of the FCTC in all nations31. Due to heavy diseases burden and high prevalence of tobacco use, there is still a long way to go for tobacco control, especially in China. Most tobacco smokers are nicotine dependent, and only 3–5% of unaided smoking cessation attempts result in successful quitting 6 to 12 months later19. Withdrawal symptoms, certain environments and social situations also lead to the high relapse rate among smokers who try to quit. Meanwhile, over 85% of residents do not have access to comprehensive treatment for tobacco dependence, and many physicians report inadequate training in tobacco treatment, and over half of adult smokers are not advised to quit smoking by healthcare providers17. So, comprehensive tobacco control measures should be implemented in the future. Tobacco control laws or regulations should be enacted and implemented under rigid monitoring. Physicians need to be trained to provide professional cessation services to tobacco users, and tobacco cessation clinics should be upgraded to serve as a vehicle to train available human resources and increase the quantity and quality of cessation services.
To our knowledge, this study is the first attempt to estimate how smoking cessation intention would be influenced by NCD comorbidity among current smokers in Shanghai, China.
Limitations
This study has some limitations. First, the sample size of current smokers was relatively small and was only selected in two districts out of the total 15 districts in Shanghai, the non-random selection of the current smokers may not represent the whole tobacco smoking population in Shanghai, limiting the generalization of our findings. Moreover, the small sample size also leads to wide confidence intervals in some subgroups. Second, the 7 types of NCDs among smokers were collected through questionnaire interviews but not extracted directly from their medical records which might cause some recall bias. The tobacco smoking cessation intention analyzed in this study was only smokers’ attitude but not their actual smoking cessation behavior, so we could not estimate the real effect of NCD comorbidity on smoking cessation intention among them. Third, except for the association between NCD comorbidity and smoking cessation intention discussed in this study, multi-facet factors were associated with the tobacco smoking quit issue, such as physicians’ advice, tobacco price increase, warning labels on tobacco package, tobacco control advertisements as well as tobacco control campaigns. Therefore, the incorporation of these aforementioned factors into comprehensive analysis would be a major step forward and should be considered in future studies.
CONCLUSIONS
The prevalence of NCD was high among smokers in Shanghai, especially in males of older age. Smoking cessation intention was strongly associated with NCD comorbidity among current smokers. Therefore, physicians should treat illness as a powerful motivation to quit among smokers and provide professional cessation services to tobacco users to help reverse the course of the tobacco epidemic.